Welcome to the Wellness Hub website! To learn more about who we are, and the work that we’ve done please click here.
Study Abstract
Keywords: long term care, pragmatic design, multidisciplinary
Authors: Christine Fahim, Jamie M Boyd, Jessica Firman, Ana Mrazovac, Vincenza Gruppuso, Keelia Quinn de Launay, Claire R. Gapare, Vanessa Bach, Nimitha Paul, Alyson Takaoka, Rosane Nisenbaum, Sharon E Straus
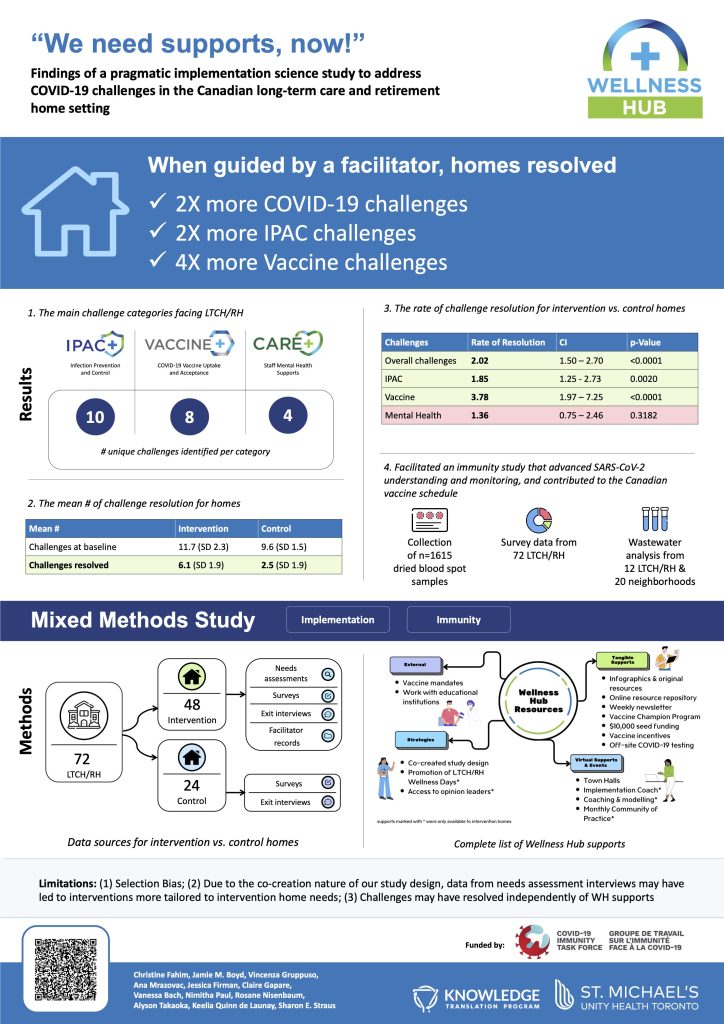
Research Aim: To describe the creation and impact of a pragmatic support program designed using co-creation methods to address COVID-19 challenges within long-term care homes (LTCH) and retirement homes (RH), while facilitating the advancement of biomedical, clinical, and implementation science.
Setting: LTCH and RH in Ontario, Canada, were one of the groups most affected by COVID-19, yet had little capacity to participate in research in the midst of their pandemic response. We formed a multidisciplinary network to define biomedical, clinical, and implementation science research questions for this population.
Methods: We interviewed 91 leaders from 47 LTCH/RH to identify their COVID-19 challenges, and used theoretical mapping to design the Wellness Hub support program. Homes were assigned to a control (self-guided resources) or intervention (facilitator-guided resources with access to community of practice) arm based on capacity and interest to participate in multidisciplinary research. We evaluated homes’ rate of challenge resolution (rate/10 challenges, rate-ratio, 95% confidence interval, CI) using a Poisson regression model. By gaining access to homes via Wellness Hub, we were also able to facilitate SARS-CoV-2 biomedical and clinical research in these settings.
Key Findings: Wellness Hub addressed infection prevention and control (IPAC), vaccine uptake, and staff well-being challenges. Challenge resolution rate for the intervention arm was 5.23 (CI:4.61-5.94) compared to the control rate of 2.59 (CI:1.99-3.38), resulting in a rate-ratio of 2.02 (CI:1.50-2.70,p=<0.0001). The intervention yielded a nearly two-fold (rate-ratio:1.85,CI:1.25-2.73,p=0.002) and four-fold (3.78,CI:1.97-7.25,p=<0.0001) higher resolution of IPAC and vaccine challenges, respectively. No significant differences were observed for well-being challenge resolution. Home type and size were not associated with resolution rate. Wellness Hub facilitated the collection of n=1,615 biological samples and sociodemographic surveys, data from 72 LTCH/RH and wastewater analysis (12 LTCH/RH, 20 neighborhoods).
Conclusion: Tailored implementation support, including facilitated coaching significantly improved resolution of COVID-19 related challenges in LTCH and RH. Implementation science provides a structured yet flexible approach to co-developing and iteratively implementing crisis-responsive interventions in long-term care and other congregate care settings.